232News
By Dr. Manal Ghazzzawi
A few days ago, I was delighted to hear that Sierra Leone is about to rollout human papilloma virus (HPV) vaccine against Cervical Cancer, with the help of international donors or non-governmental organizations (NGOs). First, I was happy to hear the good news, but after reading further, I wondered how sustainable such a roll out really is going to be. Administering 1,500 doses of the (HPV) vaccine to 10-year-old girls is a good start but we hope it continues as a nationwide routine vaccination of girls and boys aged 11-12 years, including previously unvaccinated females and males aged 13-26 years. There are still ongoing studies to ascertain whether a single shot is enough to provide a long duration of protection, like that of a 2- or 3- dose series of the HPV vaccine.
Cervical Cancer is the third most common cancer in women worldwide, and it remains a leading cause of cancer-related death for women in developing countries like Sierra Leone. Noticeably, Cervical Cancer is the second most common cancer among women in developing countries, it is only the tenth most common in developed countries. This health disparity is attributed to increased awareness, well-organized screening for HPV, appropriate infrastructure for follow up and treatment of the disease in developed countries.
Situational Analysis of Cervical Cancer in Sierra Leone
The International Agency for Research on Cancer (IARC), a body which provides HPV-related epidemiological data for WHO member states, highlights that Sierra Leone has a population of 2.33 million women aged 15 years and older who are at risk of developing cervical cancer. Current estimates by IARC indicate that every year 504 women are diagnosed with Cervical Cancer and 367 die from the disease in Sierra Leone. Though data is not yet available on the HPV burden in the population of Sierra Leone, about 4.3% of women in the general population are estimated to harbour cervical HPV-16/18 infection at any given time, and 55.6% of invasive cervical cancers are attributed to these particular strains of the virus (HPVs 16 or 18).
According to the ‘World Health Organization – Cervical Cancer Country Profiles for Sierra Leone, 2021, for primary prevention of Cervical Cancer, HPV vaccination is not included in the national vaccination schedule. For secondary prevention, as of now, there is no National screening programme for Cervical Cancer and no guidelines exist to strengthen early detection of first symptoms at primary health care level, nor does exist a clearly defined referral system from primary care to secondary and tertiary care. We are yet to have a cancer center in Sierra Leone, however when it comes to cancer treatment, there is some hope, as we have very good oncologists though few, that are making great strides when it comes to diagnosis and treatment. Sadly, patients must pay out of pocket for their anti-cancer drugs which is not cheap and therefore leads to more health disparities in Sierra Leone between those well off and poorer population. In terms of diagnostics, there are few pathology labs, but the country does not offer radiotherapy neither palliative care at primary health care facilities.
About a year ago, UNFPA, the United Nations sexual and reproductive health agency, partnered with the Chinese Embassy to provide support to the Ministry of Health by offering screening services for Cervical Cancer in nine health care facilities across the country. While these health care facilities provide screening services, they do not provide chemotherapeutic drugs. The only treatment option available at these facilities is cryotherapy which is most effective for precancerous lesion.
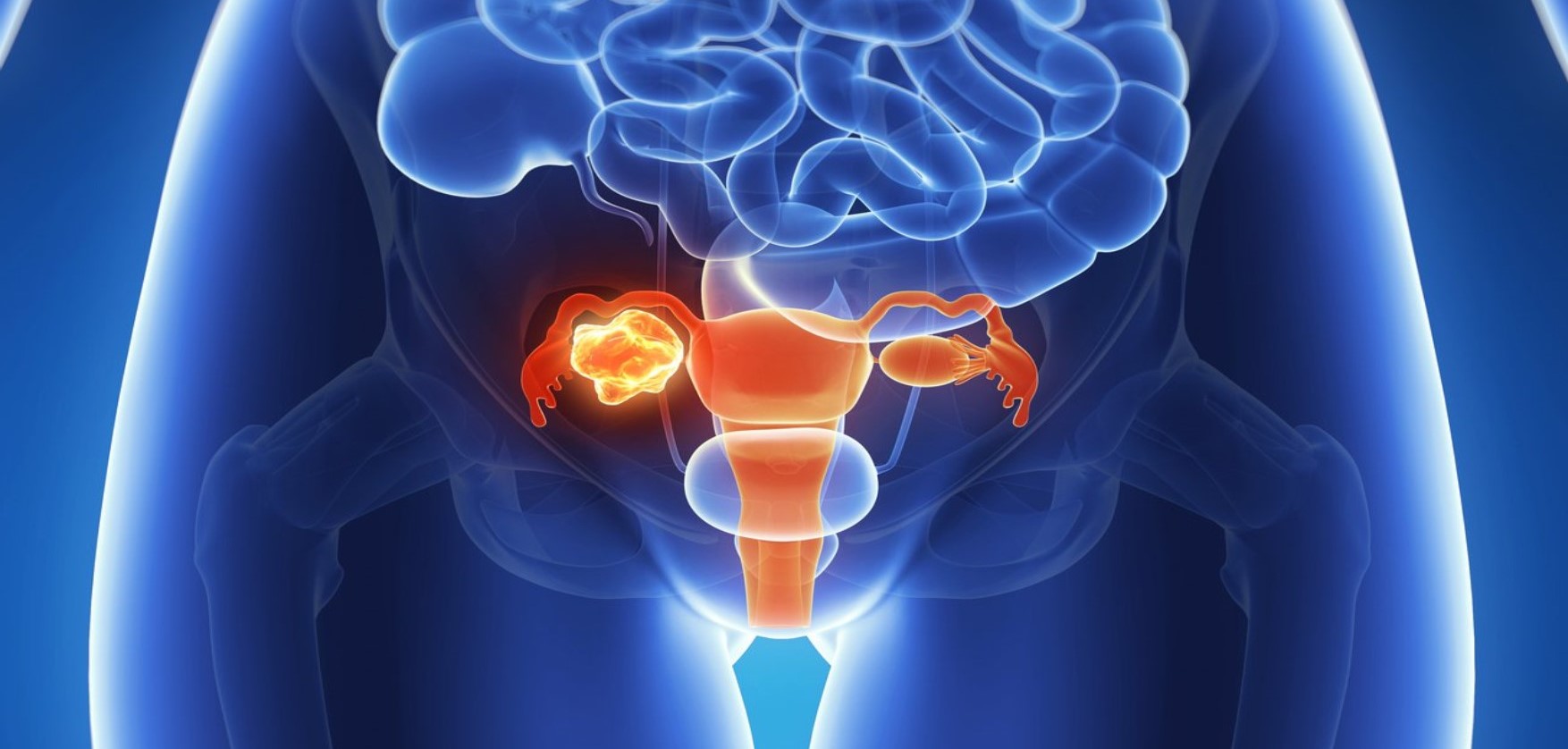
What is Cervical Cancer?
Cancer is a disease in which cells in the body grow out of control. The cancerous cells can invade and destroy surrounding healthy tissue. Cancer is always named after the part of the body where it started, even if it spreads to other body parts later. When cancer starts in the cervix, it is called cervical cancer. The cervix is considered the neck of the womb that connects the vagina and uterus (womb), and it forms part of the reproductive system.
What causes Cervical Cancer?
Nearly all Cervical Cancer is caused by the human papillomavirus (HPV). Long lasting infection with certain types of the HPV is the main cause of Cervical Cancer. HPV is a common virus that is passed from one person to another during sex. At least half of sexually active people will have HPV at some point in their lives, but few women will get Cervical Cancer. There are many types of the virus, only a certain strain/ type can cause changes in a woman’s cervix causing cancer, while other types will cause genital or skin warts.
Risk Factors
HPV is so common that most people get it at some time in their lives. HPV usually causes no symptoms, so you can’t tell whether you have it or not. For most women, HPV will go away on its own; however, if it does not, there is a chance that over time, it may cause cervical cancer. Major risk factors identified include sex at a young age, multiple sexual partners, promiscuous male partners, history of sexually transmitted diseases (STDs). HIV infection is associated with a 5-fold increase in the risk of cervical cancer, presumably because of an impaired immune response to HPV infection. Other risk factors include smoking and prolonged use of birth control pills.
Signs and Symptoms
Physical symptoms of cervical cancer may include abnormal vaginal bleeding especially after sex, vaginal discomfort, vaginal discharge with bad smell, painful urination (uncommon). Please note that the above signs and symptoms can also be related to STDs, so always speak to your doctor/gynecologist first. If Cervical Cancer is left untreated after diagnosis, the tumor can grow to affect the womb, invade the bladder and rectum (end of the large intestine) leading to constipation, blood in urine, fistula, and obstruction to urinate etc. The common sites for spreading of the tumour include lymph nodes that are outside the pelvic area, liver, lung, and bone. Ultimately, it can lead to death.
Diagnosis The Pap test and the HPV test can help prevent cervical cancer or find it early. The Pap test (or Pap smear) looks for precancerous cell changes on the cervix that might become cervical cancer if they are not treated appropriately. The HPV test looks for the virus that can cause these cell changes. According to current international guidelines, screening recommendations for specific patient age groups are as follows: < 25 years – No screening recommended 21-29 years – Cytology (Pap smear checking for cancerous cells) alone every 3 years 30-65 years – Human papillomavirus (HPV) and cytology co-testing every 5 years (preferred) or cytology alone every 3 years >65 years – No screening recommended if adequate prior screening has been negative and high risk is not present.
Management
The treatment of cervical cancer varies with the stage of the disease. For early invasive cancer, surgery is the treatment of choice. In more advanced cases, radiation combined with chemotherapy is the current standard of care.
Prevention
HPV infection is usually transmitted sexually (vaginal, anal or oral), condom use may not prevent transmission. Evidence suggests that HPV vaccines prevent HPV infection. There are existing vaccines with different strains of the virus, and some can provide cross protection against other existing strains. The Centers for Disease Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP), recommends that the vaccine be given starting from age 9 up to the age of 26 years. The HPV vaccine is normally given as a series of shots. ACIP specifies different dosing schedules, depending on the age when the vaccination series is started. Children who start the vaccine series before 15 years need only two doses to be fully protected. People who start the series at age 15 or older and people who have certain conditions that weaken the immune system need three doses to be fully protected. It’s worth mentioning that even after vaccination, screening for Cervical Cancer should continue in vaccinated women, following the same guidelines as in unvaccinated women. These vaccines do not provide complete protection against Cervical Cancer. In addition, not all vaccinated patients may mount an effective response to the vaccine, particularly if they do not receive all 3 doses. People who have an HPV infection and/or an abnormal Pap test result that may indicate an HPV infection should still receive the HPV vaccine if they are in the appropriate age group (9 through 26 years) because the vaccine may protect them against high-risk HPV types that they have not yet acquired. However, these people should be told that the vaccination will not cure them of current HPV infections or treat the abnormal results of their Pap test. Although HPV vaccines have been found to be safe when given to people who are already infected with HPV, the vaccines provide maximum benefit if a person receives them before he or she is sexually active. It is likely that someone previously infected with HPV will still get some residual benefit from vaccination, even if he or she has already been infected with one or more of the HPV types included in the vaccines. With all this in mind, the Sierra Leone Ministry of Health with the support of international partners have made a good start, but for this roll out to be effective and impactful, continued vaccination, mass awareness raising, and screening is necessary to protect our girls and women from cervical cancer.
Manal Ghazzzawi- is a Doctor of Pharmacy, a public health specialist and a consultant clinical pharmacist. She is a health entrepreneur, CEO of Citiglobe Pharmacies Ltd, and a laureate for women in Africa Entrepreneurs 2020 and has won many awards as the most outstanding pharmacist in Sierra Leone. Dr. Ghazzawi is a foundation fellow of the newly established Postgraduate College of Health Specialists in Sierra Leone.